The doctor visits involved in pursuing an evaluation for FPIES can feel both overwhelming and stressful at times. No family should have to go through this process alone!
The resources below can help guide you through the process of finding a professional to help your child, as well as help inform you of scholarly resources available for increasing your family’s own FPIES knowledge. We also understand that life goes on in between doctor visits. Tools such as the food journal tutorials, glossary of terms and Q & A, and Emergency Care information can help to support you and your family in your day-to-day life with FPIES.
New to FPIES?
Get started in the Foundation’s Toolbox for basic tools for daily living with FPIES
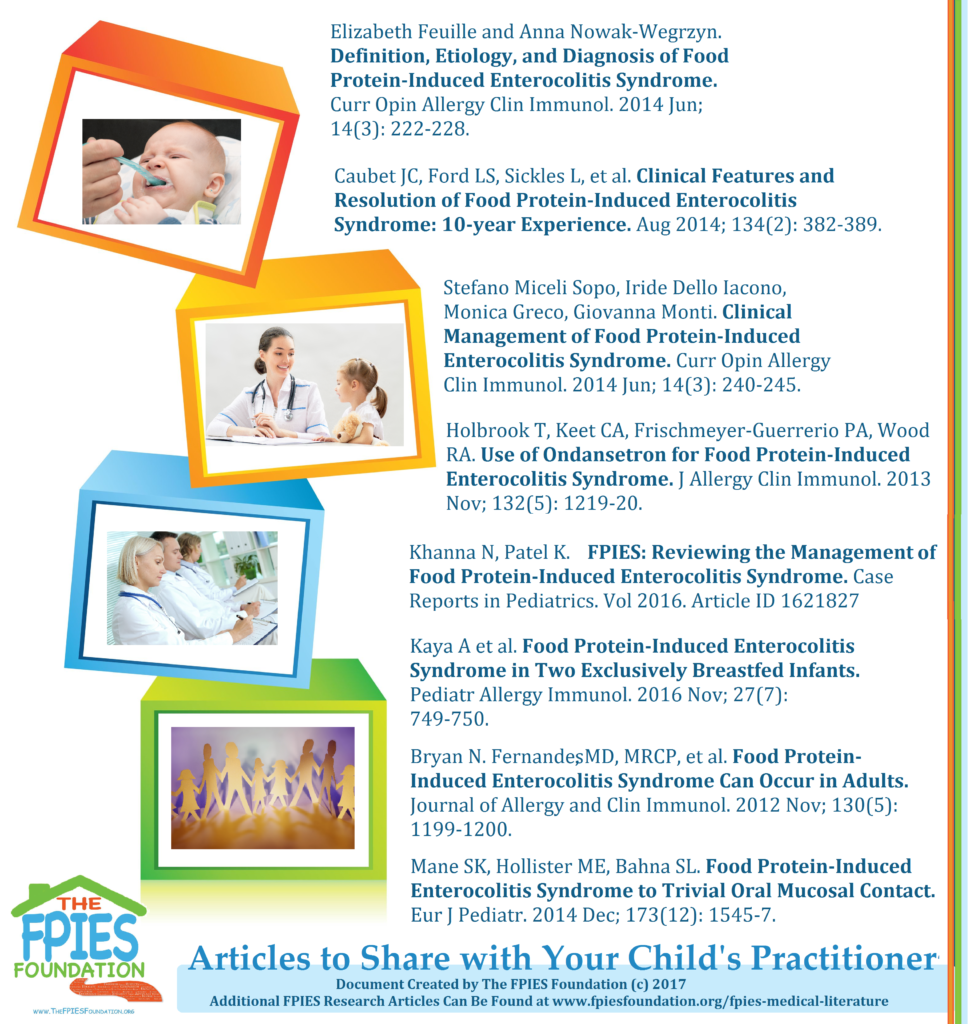
Helpful Articles to Give to Doctors
Are you concerned that your doctor may be unfamiliar with FPIES? These can help to start a conversation at your child’s next appointment about pursuing an evaluation for an FPIES diagnosis.
Locate a Healthcare Professional
Locate a Healthcare professional knowledgeable in FPIES in our free online database
Tests Your Child's Doctor May Consider
A quick overview of specific tests and what they entail in relation to an FPIES evaluation
Symptom Checker
A place to review the common symptoms involved in an FPIES reaction and the questions an evaluating physician may ask about your child’s history
Food Journals
A tool to help keep track of symptoms, your child’s diet, and any patterns that may develop between the two
Emergency Care
ER tools, including a sample ER letter written and shared by Dr.Scott Sicherer.
Recognizing Shock
From dehydration to the medical emergency of shock, use this poster to help educate family, care providers, and more on how to identify an acute FPIES reaction.
What can I expect at the first allergist and/or gastroenterologist appointment?
Be prepared to be asked many questions from your specialist. Your answers to those questions are essential because the diagnosis of FPIES is what is called a ‘clinical diagnosis’. This term, ‘a clinical diagnosis’, refers to conditions where there is no definitive laboratory tests to confirm or make a diagnosis. In these instances, the doctor depends on the child’s medical history to decide what is going on. Determining a diagnosis is essential for developing the appropriate immediate and long-term management plans.
Symptoms that occur as a result of FPIES can be similar to those caused by other medical problems. In the young child exhibiting these symptoms it is important to consider these other illnesses. They can be as devastating and need to be excluded. FPIES shares symptoms with viral gastroenteritis, bacterial sepsis, and food allergy. Other considerations include metabolic disorders and abdominal surgical emergencies. Tests are often performed to rule in or out these other diagnoses.
What the specialist needs to know-
- What happened?
- What were the symptoms experienced by the child?
- What was the time course of the child’ symptoms?
- How old was the child at the time of the event(s)?
- How many times has this happened?
- Was it the same every time?
- What was the timing from the exposure to a suspected food to the onset of the child’ symptoms?
- What foods were involved?
- What was done to take care of the child?
- How long did it take for the child to recover?
- What advice were you given about handling future events?
- What tests have been done? Specifically, if your child had any blood tests done at the time of the symptoms, can you get me those results**?
Other questions will be asked to help rule out those other medical conditions especially infection or food allergy. The selection of tests may depend on whether or not the child is currently having an acute episode or is currently well and has recovered from the event.
** During an FPIES reaction, the white blood cell count and sometimes the platelet count changes in way that can suggest FPIES– this can further assist in determining a diagnosis.
(A note from the Foundation families: it is helpful to have as much of this written down prior to your appointment as possible. Bring this with you to the specialist. Sometimes it is difficult to recall all the information during an appointment, and a information sheet they can keep allows for less time the physician spends writing- meaning more time to consult with you.)
What do I need to know about common tests used to rule out/in FPIES (i.e. types and descriptions)?
 If your child presents to the emergency department, they may evaluate your child to be sure that an overwhelming infection is not at work. Young children with a severe infection may present with the signs and symptoms shared by FPIES. Since infection is more common than FPIES, and depending on the condition of the infant or child and circumstances at the time, a physician may wish to perform tests to exclude the possibility of an infection. Additional tests may be performed once the acute reaction has passed, typically at a follow-up appointment with an allergist.
If your child presents to the emergency department, they may evaluate your child to be sure that an overwhelming infection is not at work. Young children with a severe infection may present with the signs and symptoms shared by FPIES. Since infection is more common than FPIES, and depending on the condition of the infant or child and circumstances at the time, a physician may wish to perform tests to exclude the possibility of an infection. Additional tests may be performed once the acute reaction has passed, typically at a follow-up appointment with an allergist.
CBC (complete blood count, may be performed during the ER visit):
- Results may appear to reflect an infection
- White blood cell counts and/or platelet counts in the test results may be suggestive of an FPIES diagnosis
- The obvious ‘test’ that could be performed to confirm the diagnosis of FPIES would be an oral food challenge; in a controlled clinical environment, the suspected food is reintroduced and the child is observed for symptoms of FPIES. It is important that the challenges be done only if necessary since FPIES reactions could be severe and life-threatening.
- A food challenge in a young infant who has had a significant life-threatening reaction may not be immediately necessary to make the diagnosis of FPIES, but it may be of value in the future to show that this reactivity has gone away. A food challenge for this condition would be performed in a hospital or doctor’s office.
- APT may be used to aid in diagnosis. However, it has not been universally accepted at this time and should be considered for use as a research tool rather than a standard test.
Unfortunately, there are no other blood tests or biopsies that can be done to confirm the diagnosis. If the reaction is suggestive of a IgE immediate food reaction (classic allergy), then an allergy test(s) may be performed to confirm that suspicion.

I suspect FPIES, but what do I do if my child’s doctor is not familiar with FPIES?
Because FPIES is an uncommon diagnosis, it is possible that your child’s doctor may not be familiar with it. That’s okay, and it is not an indication that you need a new physician. The vast majority of physicians are committed to ongoing medical education, and will welcome a discussion of a possible diagnosis, if you follow a few common-sense guidelines.
Let your doctor know what you’re thinking in advance. It’s never a good idea to surprise your physician with your suspicions during a routine appointment, and then expect an on-the-spot opinion. Your physician deserves some time to educate herself about FPIES before offering an opinion. Consider a phone call, letter or email to your doctor to lay the foundation for the discussion, and include a copy of a recent medical journal review article on the topic. (Here’s a suggestion: “The Current Understanding of the Immune Mechanisms of FPIES” or “Differential diagnosis of food protein-induced enterocolitis syndrome”). Ask if you can schedule an appointment to discuss the possibility of FPIES once your doctor has had an opportunity to review your child’s chart and the literature. Most physicians will be responsive to this approach.
How do I find a knowledgeable doctor to assess my child for an FPIES diagnosis?
A Board-Certified Specialist (Allergist/Immunologist or Pediatric Gastroenterologist) is an important member of the health care team caring for your child with FPIES. These fellowship-trained physicians have received special education in allergic disorders of the gastrointestinal system. A University-based medical center (especially one with a fellowship program in either Allergy/Immunology or Pediatric Gastroenterology) will have physicians who are knowledgeable about FPIES. However, many community-based physicians are also well-versed in the diagnosis and have experience managing the medical care of children with severe food allergy, including FPIES. The best way to determine if a physician feels comfortable evaluating and treating a child with FPIES is simply to call and ask if you can speak with the physician briefly before scheduling an appointment. If the doctor does not feel comfortable, managing your child’s care, he/she can most likely give you a recommendation for a trusted and respected colleague who does.
Page published: July 3, 2012. Last update: Aug.30, 2019. Copyright © 2012, The FPIES Foundation